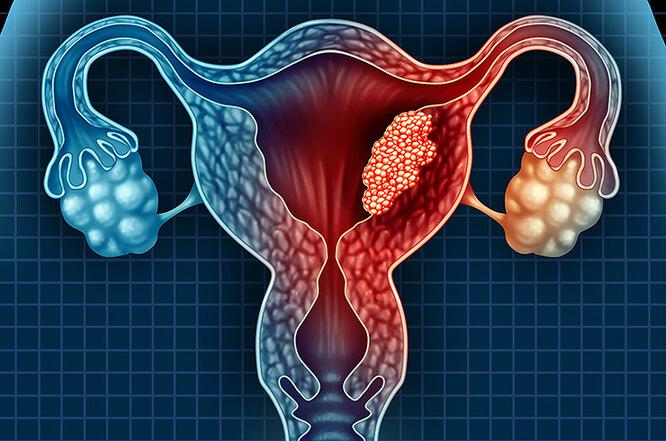
Uterine and pelvic varicose veins occur when the pelvic vein valves become weak or when the ovarian and peri-uterine connecting veins become dilated, leading to blood pooling and chronic pelvic pain, heaviness, painful intercourse, and other venous symptoms.
Interventional catheter embolization is a well-established, minimally invasive, and effective procedure used to close the diseased veins without major surgery.
When Do We Consider Catheter-Based Treatment? (Indications)
-
Chronic pelvic pain associated with confirmed pelvic venous congestion that does not improve with conservative treatment (painkillers, hormonal therapy, lifestyle modification).
-
Presence of peri-uterine varicosities or documented ovarian vein reflux on Doppler ultrasound or imaging studies (CT/MR venography or classic venogram).
-
Symptoms such as post-coital pain, pelvic heaviness or swelling, lower abdominal fullness, or visible varicose veins on the thighs/vaginal area.
How Is the Procedure Performed? (Step-by-Step Summary)
-
Pre-procedure assessment: Medical history, physical examination, Doppler/CT/MR imaging, and basic laboratory tests.
-
Catheter access: Usually through the femoral or arm vein under local anesthesia with mild sedation.
-
Direct venous imaging (venography): A contrast dye injection to map dysfunctional veins and identify reflux or obstruction.
-
Embolization: Closing the problematic veins using:
-
Coils (metallic micro-coils)
-
NBCA glue or Onyx
-
Sclerosant foam
-
or a combination, depending on anatomy and clinical need.
-
-
Final verification: Imaging to confirm complete closure of the target veins.
-
Same-day discharge: Most patients leave on the same day or after short monitoring.
Materials & Techniques Used
-
Coils: Provide safe mechanical occlusion of the vein.
-
Glue (NBCA/Onyx): Allows rapid and definitive closure.
-
Sclerosant foam: Causes controlled inflammation and gradual occlusion.
Target veins may include the ovarian veins and/or internal iliac tributaries, depending on imaging findings.
Expected Outcomes & Success Rates
-
Technical success: 95–100% vein occlusion during the procedure.
-
Clinical improvement: 60–90% reduction in pelvic pain and other symptoms, according to clinical studies and follow-up data.
Possible Risks & Complications
-
Post-embolization pelvic discomfort or localized pain — usually temporary.
-
Minor hematoma at the catheter entry site.
-
Rare complications such as infection, vein perforation, or migration of embolic material; in uncommon cases, additional procedures may be required.
-
Some insurance policies consider evidence insufficient in selected cases; final decisions depend on patient benefit and risk assessment.
What to Expect After the Procedure (Care & Follow-Up)
-
Rest for 24–48 hours with simple analgesics.
-
Avoid heavy lifting or strenuous activity for a few days.
-
Clinical follow-up after one week.
-
Doppler or CT follow-up after 1–3 months to assess venous closure and symptom improvement.
Why Choose Interventional Catheter Treatment with Dr. Mohamed Rafiq Saafan?
-
Specialized expertise in diagnosing and managing uterine and pelvic venous disorders.
-
Utilization of advanced interventional radiology techniques (coils, glue, sclerosants) with patient-specific treatment planning.
-
Comprehensive care pathway: pre-procedure evaluation, safe and precise intervention, and attentive follow-up.
💡 Why choose Dr. Mohamed Rafik Saafan's clinic?
Extensive experience in vascular surgery and diabetic foot treatment.
Utilization of the latest interventional catheterization and microsurgical techniques.
An individualized treatment plan for each patient to ensure optimal results and maximum safety.